Annual Summary of Disease Activity:
Disease Control Newsletter (DCN)
Related Topics
Contact Info
Salmonellosis, 2019
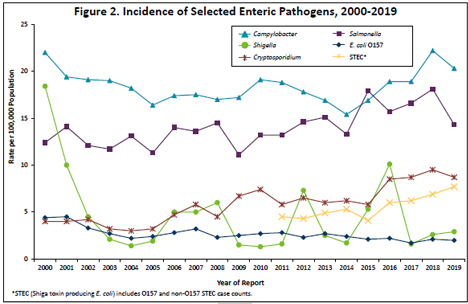
In 2019, 805 Salmonella cases (14.3 per 100,000 population) were reported. This is similar to the median annual number of cases reported from 2009 to 2018 (median, 796 cases; range, 578 to 1,009).
Of the 86 serotypes identified in 2019, 5 serotypes, S. Enteritidis (203), S. I 4,[5],12:i:- (73), S. Typhimurium (69), S. Newport (50), and S. Infantis (38) accounted for 54% of cases. Salmonella was isolated from stool in 702 (87%), urine in 47 (6%), and blood in 46 (6%) cases. Other specimen sources included wound/swab/abscess (4), pleural fluid (2), peritoneal fluid (2), pericardial fluid, and perineum.
One hundred eighty-two (23%) cases were hospitalized; the median length of hospital stay was 4 days (range, 1 to 38 days). Two culture-confirmed cases died: a 73 year-old died of adenocarcinoma 10 days after a hospitalization during which S. Poona was isolated from stool, and an 83 year-old with lymphoma died 10 days after S. Typhimurium was isolated from blood.
Of the 727 cases with known travel history, 190 (26%) had traveled internationally during the week prior to their illness onset. There were 10 S. Typhi cases; 3 traveled to India, 1 to Pakistan, 1 to El Salvador, 1 to Thailand and India, and 4 had no known international travel. There was 1 S. Paratyphi A case who had traveled to Bangladesh and Qatar.
In 2015, culture-independent tests (CIDTs) for the detection of Salmonella nucleic acid in stool became commercially available. In 2019, 49 patient specimens that were positive by a CIDT conducted at a clinical laboratory were not subsequently culture-confirmed, and therefore did not meet the surveillance case definition for inclusion in MDH case count totals.
Eighty-eight culture-confirmed cases were part of 28 Salmonella outbreaks in 2019, including 2 cases that were part of outbreaks that began before 2019. Twenty of the 28 outbreaks involved foodborne transmission, 3 involved animal contact, 2 were due to person-to-person transmission, and the transmission route was unknown for 3 outbreaks. Sixteen of the outbreaks involved cases with exposure in multiple states. The 28 outbreaks resulted in a median of 2 culture-confirmed cases per outbreak (range, 1 to 16).
Ten cases of S. Montevideo infection (including one food worker) and 1 case of S. Oranienberg infection (also a food worker) were part of a multi-state outbreak of 32 cases in 13 states that was likely associated with iceberg lettuce from fast food restaurants. The Minnesota cases were linked to two locations of a fast food burger chain. No common lettuce supplier was identified.
Nine cases of S. Bovismorbificans were part of a multi-state outbreak of 107 cases in 35 states. The national investigation determined this to be an outbreak with an unknown source, but epidemiological data among cases in Minnesota suggested that contaminated watermelon was the most likely source.
Three cases of S. Carrau infection were part of a multi-state outbreak of 137 cases from 10 states associated with pre-cut melon (including cantaloupe, watermelon, and honeydew) commercially distributed by an Indiana company. A product recall was initiated.
Three cases of S. Javiana infection were part of a multi-state outbreak of 16 cases from 8 states associated with eating a pre-packaged salad mix that contained iceberg lettuce, romaine lettuce, red cabbage, carrot, and radish.
Two cases of S. Enteritidis infection were part of a multi-state outbreak of 52 cases from 16 states that was associated with chicken; national laboratory and traceback evidence suggested a possible single facility as the source.
Two cases of S. Infantis infection were part of a multi-state outbreak that included 4 cases in Wisconsin. The implicated vehicle was vegetable trays purchased from a convenience store chain. In a separate outbreak, 1 case of S. Infantis infection was associated with a multi-state outbreak of 154 cases in 34 states that included 7 serotypes and spanned 4 years. The outbreak was associated with pig ear pet treats. No single supplier/brand/distributor was identified, and the Minnesota case’s exposures were unknown.
One culture-confirmed case a S. Newport infection was part of a multi-state outbreak of 13 cases in 7 states associated with raw tuna. A product recall was issued.
One case of S. Paratyphi B Var. L(+) Tartrate(+) infection was part of a multi-state outbreak of 12 cases in 6 states that was associated with raw tuna.
Sixteen cases of S. Enteritidis (n=14, includes a food worker), S. Infantis (n=1), and both S. Enteritidis and S. Infantis (n=1) infection were part of an outbreak at a county jail that was most likely associated with a raw, mechanically separated chicken product used in some jail meals. Leftover product tested positive for the same serotypes of Salmonella found in the human cases, and epidemiologic evidence suggested a meal that included the chicken product as the most likely source of many of the infections. Lack of temperature testing during food preparation likely contributed to the outbreak.
Seven culture-confirmed (including 2 food workers) and 2 probable cases of S. Braenderup infection were associated with a foodborne outbreak at a Minnesota restaurant. Tomato and romaine lettuce consumption were statistically associated with illness. The positive food workers may have been the source of the outbreak.
Four cases of S. Enteritidis infection were associated with an outbreak at a restaurant. The outbreak vehicle was not identified, although the environmental assessment identified multiple issues that could have led to potential contamination of either food items or equipment. Whole genome sequencing (WGS) analyses indicated that there likely was a common source of illness between cases in this outbreak and a 2018 outbreak linked to the same restaurant. In a separate outbreak, 2 cases of S. Enteritidis infection were associated with a restaurant/grocery store outbreak; no vehicle of transmission was identified.
Three cases of S. Reading infection were associated with a restaurant. The outbreak vehicle was not identified, although turkey was a plausible source, given that the outbreak cases were closely related to isolates from a recent multi-state outbreak associated with turkey. Issues were identified at the restaurant related to turkey preparation and handling that could have allowed for Salmonella survival and proliferation.
Two culture-confirmed cases of S. IV 50:z4,z23:- infection were associated with bubble tea served by a vendor at a festival. While both cases reported consuming tea from the same vendor, it is possible that they shared additional exposures at the market that were not reported, as no source of contamination was identified during the investigation.
Three culture-confirmed and 1 probable case of S. Typhi infection were associated with a fundraising event at a private home. The source of contamination and vehicle of transmission were not identified. A local health alert was issued to clinicians.
Three cases of S. Typhimurium infection were associated with horse contact. Hand hygiene training for barn crew student workers was recommended.
Two cases of S. Saintpaul infection were both inpatients at the same hospital facility prior to specimen collection. The route of transmission was unknown.
Two cases of S. Infantis infection were part of a person-to-person outbreak at a childcare center. One culture-confirmed case and 2 probable cases of S. I 4,5,12:i:- infection were part of a person-to-person outbreak at an in-home child care.
One culture-confirmed and 5 probable cases of S. Reading infection were associated with a game feed event in Iowa. The implicated vehicle was smoked turkey sourced from a Minnesota producer.
One culture-confirmed case of S. Paratyphi B Var. L(+) Tartrate(+) was part of an outbreak associated with a restaurant in Kentucky.
One culture-confirmed case of S. I 4,5,12:i:- infection was part of an outbreak of salmonellosis and rotavirus gastroenteritis associated with a private gathering in Wisconsin. The transmission route was unknown.
One culture-confirmed case and 1 probable case of S. Enteritidis infection were part of a foodborne outbreak at a Wisconsin restaurant associated with steak tartare.
One case of S. Javiana infection was associated with a family reunion outbreak in Arkansas with an unknown transmission route.
One case of S. Javiana infection was part of a foodborne outbreak at a hotel in New York City.
Among the 2 Salmonella cases in 2019 who were part of outbreaks that began before 2019, 1 (S. Typhimurium) was part of a 2018 outbreak associated with hedgehogs, and 1 (S. Infantis) was part of a 2018 national outbreak associated with chicken.
- Find up to date information at>> Salmonellosis (Salmonella)
- Full issue>> Annual Summary of Communicable Diseases Reported to the Minnesota Department of Health, 2019