Annual Summary of Disease Activity:
Disease Control Newsletter (DCN)
Related Topics
Contact Info
Salmonellosis, 2018
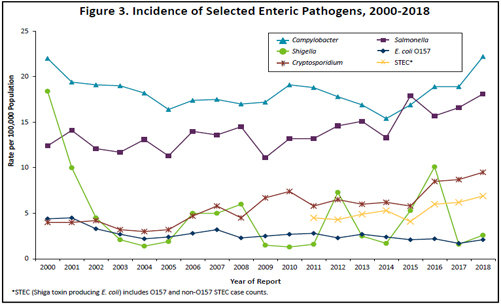
In 2018, 1,009 Salmonella cases (18.1 per 100,000 population) were reported. This is a 31% increase from the median annual number of cases reported from 2008 to 2017 (median, 768 cases; range, 578 to 975), and the highest number of Salmonella cases reported since at least 1988.
Of the 99 serotypes identified in 2018, 5 serotypes, S. Enteritidis (264), S. Typhimurium (104), S. I 4,[5],12:i:- (88), S. Infantis (42), and S. Saintpaul (40) accounted for 53% of cases. Salmonella was isolated from stool in 860 (85%), urine in 87 (9%), and blood in 54 (5%) cases. Other specimen sources included abscess (3), wound (2), cerebrospinal fluid, peritoneal fluid, and synovial fluid.
Two hundred forty (24%) cases were hospitalized; the median length of hospital stay was 4 days (range, 2 to 60 days). Five culture-confirmed cases died: a 75 year-old died of septic shock and Salmonella bacteremia; an 86 year-old died of chronic obstructive pulmonary disease and community-acquired pneumonia, with contributing Gram-negative sepsis secondary to S. Enteritidis and E. coli urinary tract infection; a 72 year-old died of acute respiratory distress syndrome and Salmonella bacteremia; a 99 year-old died of “natural” causes 6 days after S. Enteritidis was isolated from urine; and, an 80 year-old who of multiple causes including sepsis and Salmonella colitis.
Of the 912 cases with known travel history, 141 (15%) had travelled internationally during the week prior to their illness onset. There were 4 S. Typhi cases associated with travel to or immigration from India, Liberia, Guatemala, and Nepal. There were 3 S. Paratyphi A cases; 2 travelled to India and 1 had no known international travel. There were 4 S. Paratyphi B cases; 1 was not able to be interviewed, and 3 had no known travel history.
In 2015, culture-independent tests (CIDTs) for the detection of Salmonella nucleic acid in stool became commercially available. In 2018, 73 patient specimens that were positive by a CIDT conducted at a clinical laboratory were not subsequently culture-confirmed, and therefore did not meet the surveillance case definition for inclusion in MDH case count totals.
One hundred sixty cases were part of 20 Salmonella outbreaks in 2018, including 18 cases that were part of outbreaks that began in 2015 or 2017. Fifteen of the 20 outbreaks involved foodborne transmission, 2 involved animal contact, and 3 were due to person-to-person transmission. Ten of the outbreaks involved cases in multiple states. The 20 outbreaks resulted in a median of 4 culture-confirmed cases per outbreak (range, 1 to 32).
Eleven culture-confirmed and 5 probable cases of S. Enteritidis infection were associated with a restaurant outbreak. The vehicle of transmission was smoked chicken. The most plausible explanation for the outbreak was undercooking of the smoked chicken that was served on the implicated meal date. Six culture-confirmed cases of S. Infantis (n=3), S. Enteritidis (n=2), and S. Typhimurium (n=1) infection were associated with a second restaurant outbreak. Three of the infections were from two food workers. A single outbreak vehicle was not identified. Thirty-two culture-confirmed cases and 1 probable case of S. Enteritidis infection were part of an extended outbreak at a third restaurant. The investigation included four rounds of environmental health interventions, including three rounds of employee stool specimen submissions. A single outbreak vehicle was not identified. The outbreak was ongoing for 5 months, indicating there was a reservoir for the bacteria in the restaurant; this reservoir could have been food workers, the environment, or both. Two culture-confirmed cases of S. Enteritidis infection were part of an outbreak at a fourth restaurant. The vehicle and source of contamination were not identified. Two culture-confirmed cases of S. I 4,[5],12:i:- infection were associated with an outbreak at a fifth restaurant. The vehicle and source of contamination were not identified. Six culture-confirmed cases of S. Thompson infection were part of a sixth restaurant outbreak. One of the cases was a food worker; however, the outbreak vehicle was not identified.
Two culture-confirmed cases of S. Enteritidis infection were reported from a child care center; the outbreak was suspected to be caused by person-to- person transmission. Two culture-confirmed cases of S. I 4,[5],12:i:- infection were associated with an outbreak at a second child care center. Two culture-confirmed cases of S. Typhimurium infection were identified who attended the same in-home child care facility.
Four culture-confirmed and 1 probable case of S. Typhimurium infection were part of a multi-state outbreak of 265 cases in 8 states associated with commercially produced chicken salad sold at grocery stores. Seven culture-confirmed cases of S. Enteritidis infection were associated with raw breaded chicken products that were distributed primarily through a pop-up pantry program in unlabeled bags. The outbreak included 6 cases in Wisconsin, and chicken from case households in both states tested positive for the outbreak strain. Twenty-five culture-confirmed and 11 probable cases of S. Sandiego (n=23) and S. IIIb 61:l,v:1,5,7 infection (2 cases) were linked to a multi-state outbreak of 101 cases in 10 states that was associated with commercially distributed pasta salad. These numbers include 1 case who was positive for both serotypes and was therefore counted as 2 cases. A subset of the Minnesota cases attended a wedding where the pasta salad was served. The pasta salad was produced at a central commissary kitchen in Nebraska; the source of contamination was not identified.
Twenty culture-confirmed cases of Salmonella infection (S. Enteritidis, n=17; S. Indiana, n=2; and S. Montevideo, n=1) were part of a multi-state outbreak linked to live poultry contact. Nationally, 334 cases from 47 states in this outbreak were infected with 6 Salmonella serotypes. Four culture-confirmed cases of S. Infantis infection were part of a multistate outbreak of 129 cases in 32 states. Laboratory and epidemiological evidence suggests that the outbreak strain occurs widely in live chickens and a variety of raw chicken products.
Four culture-confirmed cases of Salmonella infection (S. Montevideo, n=2; S. Cubana, n=2) were part of a multi-state outbreak associated with alfalfa sprouts. One culture-confirmed case of S. Mbandaka infection was linked to a multi-state outbreak of 135 cases in 36 states. The implicated product was a dry breakfast cereal; multiple food samples also tested positive, and the company issued a recall. Five culture-confirmed cases of S. Typhimurium infection were included in a multi-state CDC-defined outbreak that may have been associated with spices. Two culture-confirmed cases of S. Newport infection were linked to a multistate outbreak of 403 cases from 30 states. The implicated vehicle was raw ground beef from a single supplier; the supplier subsequently recalled approximately 12 million pounds of beef products. Two culture-confirmed cases of S. Typhimurium infection were associated with hedgehog contact; these cases were part of a multi-state outbreak that included 17 cases in 11 states. Hedgehogs were purchased from a variety of sources, including hedgehogs bred in-house in Minnesota, and some were positive for the outbreak strain of Salmonella. Two culture-confirmed and 2 probable cases of S. I 4,[5],12:i:- infection were associated with a pig roast event. A single vehicle was not identified.
Among the 18 Salmonella cases in 2018 who were part of outbreaks that began before 2018, 2 (S. Heidelberg) were part of a 2015 outbreak associated with dairy calves, 2 (S. Infantis) were part of a 2017 child care outbreak, 2 (S. Montevideo) were part of a 2017 casino outbreak in Iowa, and 12 (S. Paratyphi B var. L(+) tartrate(+), n=7; S. Thompson, n=3; S. Okatie, n=1; and S. Weltevreden, n=1) were part of a multi-state outbreak associated with kratom. Kratom is a product derived from a tree endemic to Southeast Asia having opioid or stimulant properties.
- For up to date information see>> Salmonellosis (Salmonella)
- Full issue>> Annual Summary of Communicable Diseases Reported to the Minnesota Department of Health, 2018