Trauma Experienced by Afghan Refugee Children
Trauma-informed Care for Afghan Refugee Children
Background
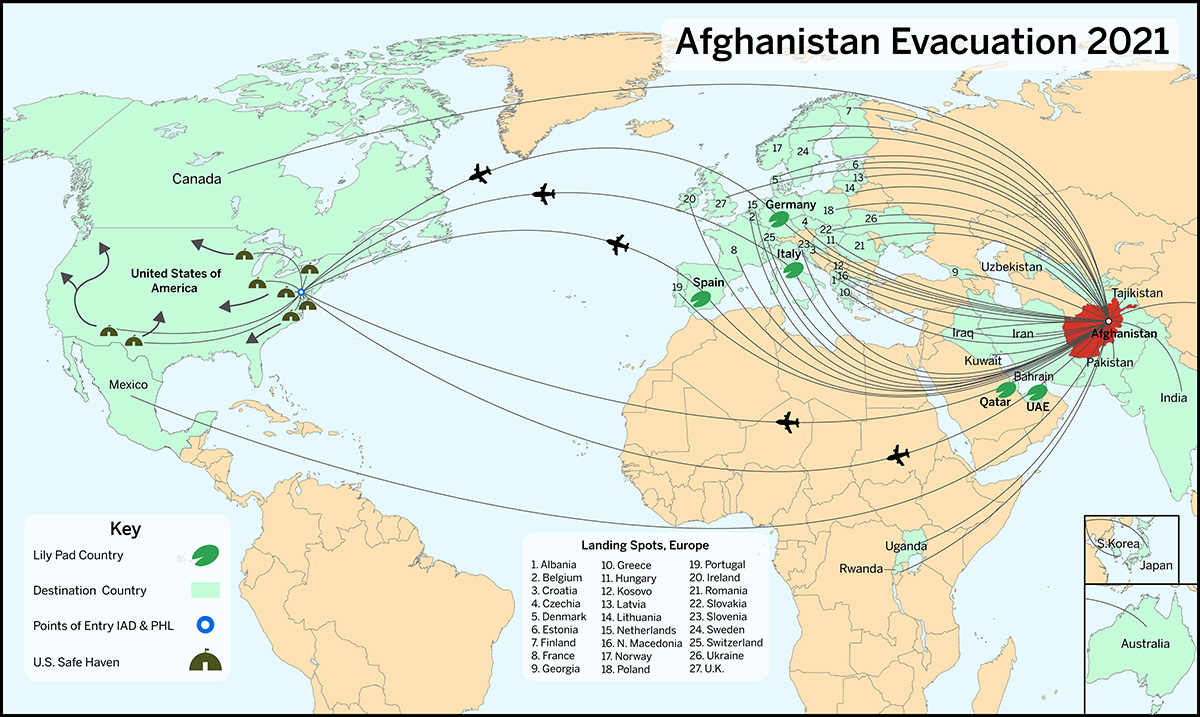
The USA War in Afghanistan against the Taliban lasted 20 years from 2001-2021. It was the longest war in the history of the United States. The Taliban returned to power in 2021 which coincided with a rapid withdrawal of U.S. troops and personnel. Over 122,000 people were airlifted abroad from Kabul airport including 97,000 Afghans. 1 According to the Council on Asian Pacific Minnesotans, more than 1200 Afghan refugees have resettled in Minnesota with more than 85% of them living in Hennepin and Ramsey counties. The evacuees make up 386 family units with 46% of arrivals under 15 years of age. 2 The purpose of this report is to examine the trauma experienced by these families and to identify screening and assessment tools that may be of value to the providers in Minnesota seeing these children.
Exposure to trauma by refugee children increases the likelihood of both immediate and lifelong potential for serious health problems. As health care providers have grown aware of trauma’s impact, they are realizing the value of trauma-informed approaches to care. Trauma-informed care (TIC) acknowledges the need to understand a patient’s life experiences in order to deliver effective care. In addition, TIC has the potential to improve patient engagement, treatment adherence, health outcomes, and provider and staff wellness. 3
Trauma informed care acknowledges that trauma may occur along the “Arc of Migration” experienced by the family and their children as depicted in the figure below.4
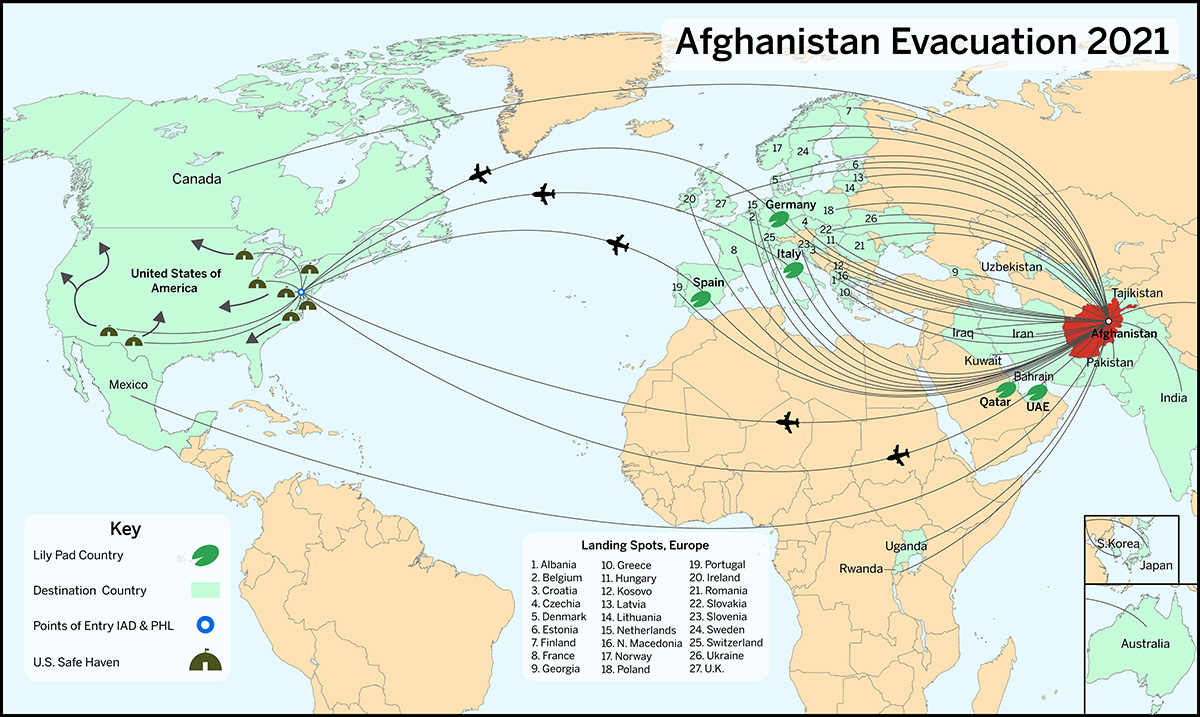
This includes the firsthand trauma experienced in their home country during the years of war and conflict including frequent injuries to and loss of a loved ones. Secondly, it also includes the trauma experienced from evacuation and transit from Afghanistan to a new home country for resettlement. Finally, the challenges experienced after their arrival in a new country can also be traumatic. Even when refugees are able to safely relocate to a new country, the resettlement process may expose them to adverse outcomes of racism, islamophobia, xenophobia, and, more broadly speaking, a “deficit mindset” held by those who serve them. The significant mental health conditions may include emotional and behavioral difficulty as well as Post Traumatic Stress Disorder (PTSD). 5
Emotional & Behavioral Health Conditions Associated with Trauma
Emotional and behavioral disorders may be seen in Afghan refugee children. Traumatic experiences may contribute to both internalizing (anxiety, depression) and externalizing (hyperactivity, opposition/defiance, aggression) behaviors or both. The provider should determine the optimal approach for testing and/or referral. A referral to a therapist who is adept at trauma informed care and with working with refugee children is certainly appropriate.
There is a broad body of research that has shown that traumatic and stressful experiences by refugee children are associated with internalizing behaviors such as anxiety and depression. Derluyn and colleagues identified that adolescent refugees who had been separated from their parents had significantly higher depression scores. 6 Jackoben and colleagues found major rates of depression of at 9.4% and anxiety disorder at 3.9%. 7 Sanchez-Cao revealed that even with high rates of depression in unaccompanied refugee minors they were frequently not in contact with mental health services. 8 Both the Jackoben and Sanchez-Cao teams included Afghan refugee minors as part of their assessments. Externalizing problems appear to be less likely in unaccompanied refugee youths than internalizing problems. 9
Stress, Trauma, & PTSD in Afghan Refugee Children
It is important to remember that children are resilient and can surprisingly cope with exposure to trauma. However, if while during an initial clinical encounter the parent mentions concerns and/or you as a provider observe behaviors that are suggestive of a child experiencing significant stress and trauma further screening may be appropriate. However, screening should not necessarily be undertaken on an initial intake visit but is more appropriate at a follow-up visit.
There is a litany of screening and assessment tools for stress, trauma, and PTSD in children. Some are appropriate for the primary care setting and others require training by the clinician or other health personnel such as psychologists, social workers, psychiatrists, etc.